The most prevalent cause of lower extremity ulcers is venous, often known as stasis ulcer. Inflammatory mechanisms that result in leukocyte activation, platelet aggregation, endothelial damage, and intracellular edema are all possible causes of venous ulcers. Old age, deep venous thrombosis, past leg injuries, obesity, and phlebitis are the key risk factors for venous ulcer formation. Venous ulcers are often irregular, shallow, and found over bone prominences on examination. The ulcer foundation usually contains granulation tissue.
Lower extremities varicosities, edema, venous dermatitis, and lipodermatosclerosis are all common findings associated with venous ulcers. They are also frequently recurrent, and an open ulcer can last anywhere from a few weeks to several years. Cellulitis, osteomyelitis, and malignant transformation are all serious consequences. Large ulcer size and duration are both poor prognostic indicators. Pentoxifylline, dressings, compression therapy, and therapy are all evidence-based treatments for venous ulcers.
Symptoms:
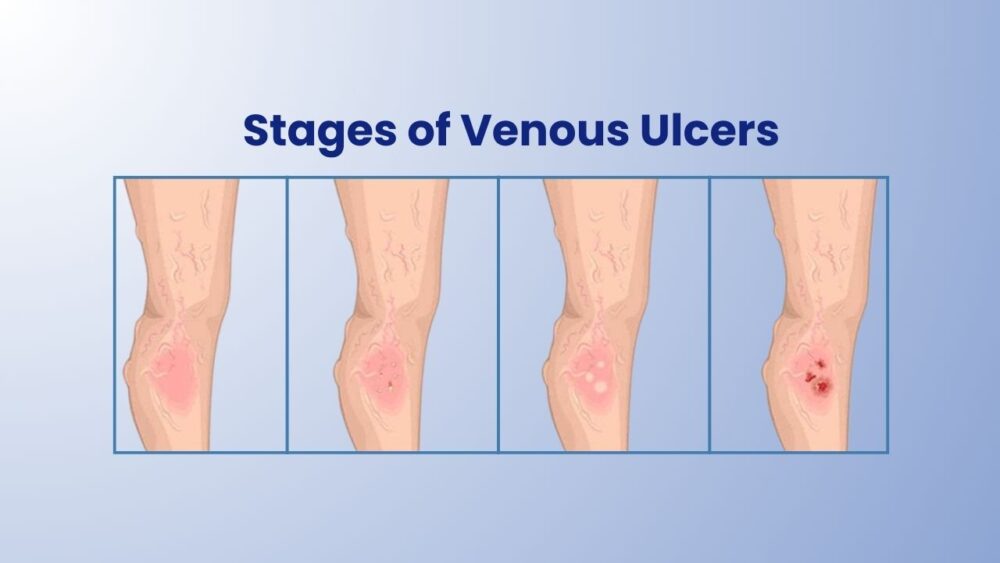
Skin that turns dark red or purple over the area where blood is spilling out is the first sign of a venous skin ulcer. It's also possible for the skin to grow thick, dry, and irritating.
An ulcer can occur if left untreated. It's possible that the ulcer is painful. The infection may generate an odour, and pus may ooze from the wound if the wound becomes infected. It's also possible that the region around the wound will be more painful and red.
Venous leg ulcers are open, often painful, sores in the skin that take more than 2 weeks to heal. They usually develop on the inside of the leg, just above the ankle.
If you have a venous leg ulcer, you may suffer from:
- swollen ankles (oedema)
- hardened skin around the ulcer, which may make your leg feel hard
- discoloration and darkening of the skin around the ulcer
- a heavy feeling in your legs
- aching or swelling in your legs
- swollen and enlarged veins on your legs (varicose veins)
- red, flaky, scaly, and itchy skin on your legs (varicose eczema)
- an unpleasant and foul-smelling discharge from the ulcer
Caring for Venous Leg Ulcer
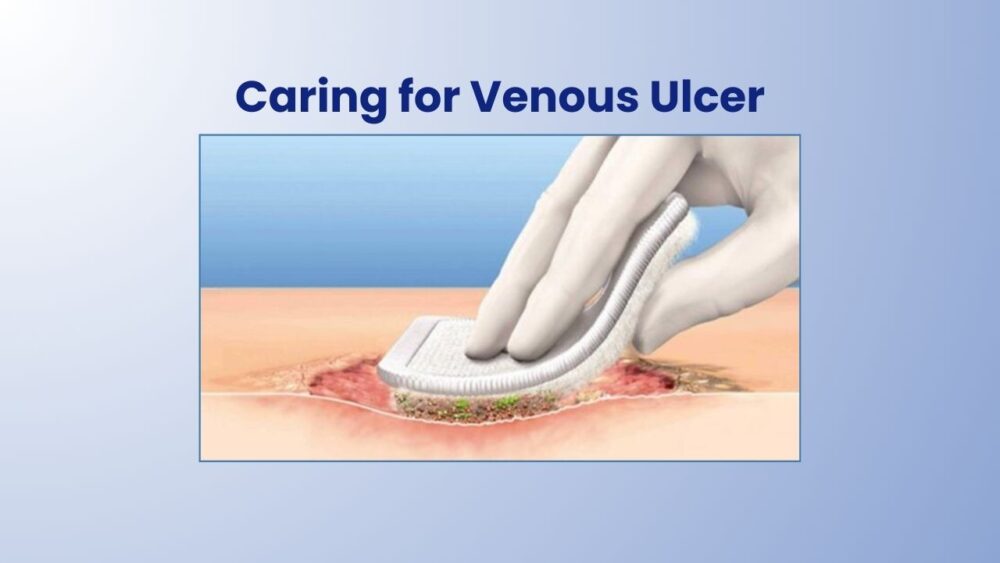
Venous ulcers require special attention and treatment to avoid infection and recovery. Your healthcare physician should check any venous ulcers as soon as possible.
The ulcers may require treatment that focuses on the circulation or venous issues that are generating the ulcers. It could also imply removing some of the tissue around the incision. It's possible that you'll be requested to:
- Clean the wound regularly
- Apply a dressing to the ulcer
- If you want to prevent or treat an illness, avoid using products that cause skin sensitivity.
- Wear compression stockings to avoid blood pooling in the legs and speed healing
- Use an antibacterial ointment or another topical drug to prevent or cure an infection
- Take oral antibiotic medicines to prevent or treat an infection
- Have allergy testing done
Compression wraps, which keep blood pumping back up to your heart, can also help ulcers heal faster. To close the opening in the skin, surgery or a skin graft may be required in some circumstances.
What Causes Venous Leg Ulcer?
Venous ulcers develop when the skin on your leg breaks, commonly around the ankle.
The veins in the leg, which are supposed to return blood to the heart, may not be doing their job properly. That's because the valves that restrict blood from flowing back into the veins aren't operating properly.
This blood backflow causes higher pressure at the limb's end. When this happens, the skin becomes weaker, making it more difficult for a cut or scrape to heal. They're more common in bony places like your ankle.
Who is Most at Risk from Venous Leg Ulcer?
Several factors can raise your chances of getting a venous leg ulcer, including:
- Obesity or being overweight increases the pressure in the veins of the legs.
- If you have trouble walking - this might weaken the calf muscles, affecting leg vein circulation.
- Previous deep vein thrombosis (DVT) – blood clots in the legs can damage vein valves.
- Varicose veins – swollen and enlarged veins produced by faulty valves.
- A past leg injury, such as a broken or fractured bone, can induce DVT or make walking difficult.
- Prior leg surgery, such as a hip or knee replacement, might make it difficult to move around.
- Increasing age – people find it more difficult to move around as they become older, especially if they have arthritis.
Diagnosis
If a venous leg ulcer is detected, your doctor will perform a full physical exam, including a blood pressure check in your arm and ankle. The foundation of successful leg ulcer care is an accurate diagnosis. The diagnosis is usually made based on the patient's statement of how the ulcer started and the results of a physical examination. Additional tests may include the following:
Ankle-brachial index test: Blood pressure cuffs are placed on the arms and ankles during this procedure. To listen to the blood flow and assess the blood pressure, handheld ultrasound equipment known as a 'Doppler' is used. This aids doctors in determining whether or not there is a reduction in blood flow to the lower legs and feet.
Ultrasound: An ultrasound instrument can test blood pressure in various parts of your arm or leg, allowing your doctor to see if you have any blockages and how rapidly blood flows through your lower leg arteries.
Infection should be checked on venous leg ulcers. Antibiotics may be required based on the results of wound culture. In addition, the tests listed p may be used:
Imaging tests: X-rays, magnetic resonance imaging (MRI), and bone scans can all be used to detect bone infection and evaluate whether medical treatment or procedure is required to treat infected venous ulcers completely
Preventing venous ulcers
To avoid venous ulcers, you must first avoid vein issues. This can be accomplished by adopting healthy habits that promote blood flow in your legs. These lifestyle modifications can help you improve your circulation and lower your risk of venous ulcers:
- Avoid smoking
- Lose weight if you're overweight or obese
- Stay at your ideal weight
- Get plenty of regular exercises
- Move around often
- For a brief period, raise (elevate) your legs, especially if you've been standing all day.
Compression stockings can also be beneficial. They are able to:
- Prevent blood from pooling in your legs
- Help you avoid significant swelling
- Reduce your risk for venous ulcers
Treatment and Recovery
Venous leg ulcer treatments include controlling the high pressure in the leg veins and treating the ulcer.
Controlling PressurePatients with venous leg ulcers must keep their swelling under control. Leg elevation, with the feet at or above the level of the heart, can help reduce swelling multiple times throughout the day and while sleeping. Legs are frequently wrapped in compression wraps or bandages. Depending on the quantity of fluid leaking from the ulcer, they can be changed as frequently as several times a day or as infrequently as once a week. Elastic compression stockings may be indicated once the leg ulcer is smaller or virtually healed. Compression stockings are fitted to fit the legs and are often worn throughout the day. Patients with significant edema may be prescribed a venous pump.
Treating UlcerThe initial step in treating a venous ulcer is to remove any dead tissue surrounding the sore, followed by the use of a specific dressing to promote healing. Once a week, the dressing will need to be changed. A compression stocking may be used over the dressing at times. A compression bandage on an ulcer is unpleasant for the first few weeks. Your doctor will prescribe a pain treatment that is appropriate for you. Leg ulcer discomfort will reduce as the ulcer heals.
SurgeryPatients with varicose veins who have acquired poorly healing wounds require more sophisticated wound care and treatment. New varicose vein treatment alternatives are less invasive, require little anaesthetic, and can be done in the comfort of a doctor's office or an outpatient surgical centre. Treatment options vary depending on which vein groups are generating symptoms, however, they can include:
- Endovenous ablation: This technique is performed as an outpatient procedure. In the great or small saphenous vein, a catheter is placed. The vein is heated with radio waves or a laser after numbing medicine is injected into the skin along the area of the vein to be treated. This ablation (heating) procedure takes about 45-60 minutes. Blood that is used to pool in the treated superficial vein is diverted into the deep vein system by nature. Patients get relief in a few weeks or it might take a few months. Following the surgery, patients are urged to walk as soon as possible. Anti-inflammatory drugs like ibuprofen are used to treat pain, which is rarely severe. A week after the surgery, a follow-up visit will be scheduled to check for any blood clots, and medication may be recommended to help treat the clot.
- Ambulatory phlebectomy: This treatment for branch varicose veins can be done in the office or as an outpatient surgery. The doctor marks the veins that will be removed after the patient stands for several minutes to allow the veins to check for any blood clot which can happen rarely. Medicine is injected into the skin along the course of the veins to be treated once the veins have been marked and confirmed by the patient. The veins are removed using a small hook through very small incisions, or nicks, in the skin. No stitches are required because the incisions are so small that patients are allowed to walk right away. The majority of people do not require pain medication, but anti-inflammatory medication is sufficient when they do.
- Sclerotherapy: This treatment for branch varicose veins can be done in the office or as an outpatient surgery. In smaller veins the solution is injected with a tiny needle filled with a liquid that sclerosis (or shuts) the vein. There is no need for anaesthetic or numbing medication for this procedure. This treatment is best for treating smaller veins (also known as spider veins).
Complications
A venous leg ulcer can cause a number of major health issues, such as:
Loss of mobility: A venous leg ulcer can be unpleasant, limiting activity and aggravating the condition.
Infection: Venous ulcers are very susceptible to infection. Blood poisoning or a bone infection can occur if the infected venous ulcer is not treated.
Dr Nellie is one of the very few female phlebologists in Australia and New Zealand, having earned her fellowship in the same field. Dr Yazdani has Certified skills in Advanced Ultrasound in Phlebology, she has been treating patients for more than 17 years with no or minimal adverse effects.
Visit Melbourne’s highly rated vein clinic i.e. Melbourne Varicose Vein clinic today for any of your painful vein conditions.