Varicosities veins, also known as vulvar varicose veins, are not a regular subject of conversation among pregnant women, but they should be. Vulvar varicosities are estimated to afflict between 4% and 10% of pregnant women, but the true figure is likely to be significantly higher because many women do not report or are diagnosed because they are too ashamed to discuss their symptoms with their health care provider. Weak Valves are not the only reason for varicosities veins
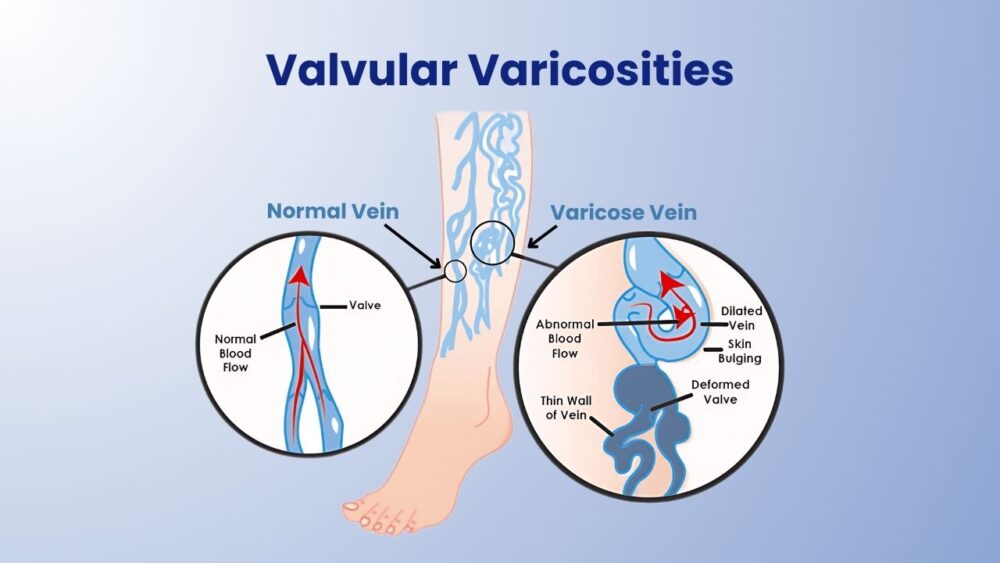
Small crescent-shaped flaps of tissue called valves are strewn throughout your veins to assist prevent blood backflow. These valves are inclined towards the heart and project from the innermost layer of the vein wall to the core of the vein in the direction of venous blood flow. They work passively, like swinging doors, because they lack the muscles to open and close them. When blood rushes through a valve, it pulls the valve open, and when the blood flow slows, the valve closes.
Collagen is a protein that makes up vein valves. Collagen properties differ slightly from person to person, with some people making more flexible collagen and others producing a stiffer form. If you fall into the latter category, your valves may be more prone to wear and strain, and damage.
- Varicose veins of the vulva, also known as vulvar varicosities, are a type of varicose vein that causes swelling of the vaginal outer lips due to blood pooling in the veins. Varicosities veins are not only unsightly, but they can also be unpleasant, causing the vulva to ache and hurt.
- Some women will have apparent varicose veins around the vulva, inner thighs, and behind, while others will have no visible symptoms but still experience pain.
- Women's pain around the pelvic and/or lower back is the most prevalent symptom, which they describe as a dull aching. The pain usually worsens over the day, as long periods of standing or sitting aggravate the disease.
- Pain can also occur during sexual activity and before and during menstruation.
- Varicose veins in the pelvic might also make it necessary to urinate more frequently.
- The valve flaps may no longer be able to reach each other in the closed position when the vein walls weaken and enlarge with age. This causes blood to seep or regurgitate.
- The emotional side of the problem can be a contributing role in prenatal anxiety and depression, which is why we need to discuss it.
Vein health necessitates physical activity. When you tighten your leg muscles, they gently compress the veins, allowing blood to flow more freely. Having a desk or standing work that demands you to be sedentary for long periods of time diminishes the beneficial effects of muscle movement, resulting in sluggish blood flow. This causes venous hypertension, which causes the veins to enlarge and the valves to leak.
It's crucial to remember that vulvar varicosities are unlikely to cause complications during pregnancy and delivery, and they usually go away on their own within six weeks of your baby's birth. Because these veins have a minimal blood flow, any bleeding would be quickly managed. As usual, seeing a health care expert for peace of mind and to ensure that your health is not affected should always be your first step, especially now that you are responsible for that beautiful life developing in your womb.
The effects of female hormones on vein valves are considerable. The walls of the veins and the valve tissue weaken when progesterone is present. High levels of progesterone, such as those found during pregnancy, can cause veins to dilate and valves to leak. Progesterone excess might cause the valves to become excessively flexible and fail to seal properly.
Estrogen has anti-inflammatory properties that help to preserve vein valves from injury. The number of oestrogen receptors in the veins has been observed to rise as venous insufficiency increases, and this is true for both men and women.
A blood clot in the leg can damage the valves, causing blood flow to be obstructed. The valve finally loses its way and opens in the wrong direction as backpressure accumulates, causing damage. A blood clot on a valve can also create scarring, which makes it difficult for the valve to open and close appropriately.
Vein valves can also be damaged by a past accident or injury to the legs, surgery on the legs, or a disease process that affects the circulation.
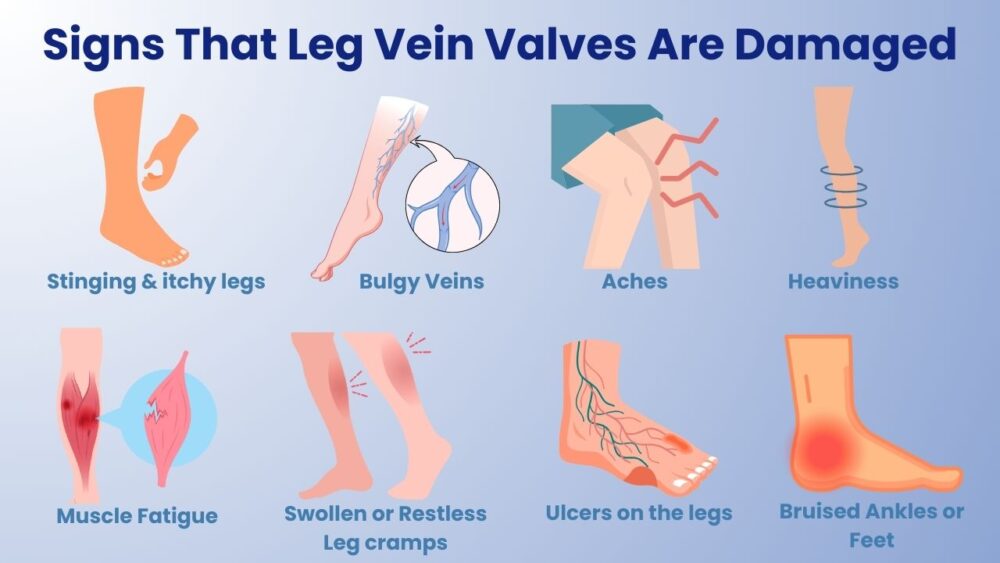
What Are the Signs That My Vein Valves Have Been Damaged?
The circulation in your legs will be severely hampered as the number of damaged valves increases. This illness, also known as venous insufficiency. The following are some of the symptoms of venous insufficiency, which can range from minor to severe:
- Stinging & itchy legs
- Bulgy Veins
- Aches
- Heaviness
- Muscle Fatigue
- Muscle spasms or leg cramps
- Legs or ankles that are swollen
- Legs that are restless, especially at night
- Ulcers on the legs
- The skin around the ankles has a dark, bruise-like appearance.
How are varicosities veins treated?
You can address swollen feet & ankles, restless legs especially at night, leg ulcers, and venous insufficiency symptoms with a few basic self-care techniques. Compression stockings are a good option for preventing blood pooling and reducing swelling and achiness. If you want higher amounts of compression, these are available over-the-counter or by prescription.
Walking is one of the finest forms of exercise you can do for your vein valves, and it is one of the best forms of exercise you can do for your vein valves. Walking, which is sometimes referred to as the "ideal" exercise, is effective for people with faulty vein valves because it activates the muscle pump in the legs, which helps to prevent blood pooling and feelings of heaviness. Swimming, dancing, or any other sort of exercise that gets your legs moving is an option if you prefer a different activity. Elevate your legs in between workouts to benefit from gravity's help.
- If your symptoms have worsened or you simply want to get rid of your compression stockings for good, there are a number of minimally invasive procedures that can be done in the clinic with only local anesthesia.
- VenaSeal is a long-term treatment for varicose veins that involves injecting an adhesive into the problematic veins, which seals them up and redirects blood flow to healthy veins.
- ClosureFast uses advanced radiofrequency ablation (microwaves) to treat and close problematic veins, and blood is subsequently diverted to healthy veins.
Dr. Yazdani is a very highly rated vein expert to treat Valvular Veins. At our clinic, the environment is very friendly & comfortable because we understand your anxiety and we will try to address all your questions at the very first consultation.
Visit Melbourne Varicose Vein Clinic today for Valvular Vein Condition, Book your appointment online or call us to help you reach Dr. Nellie.